Lab 9 (ƒ 10) - Cranial Nerve Nuclei and Brain Stem Circulation
Review of Blood Supply
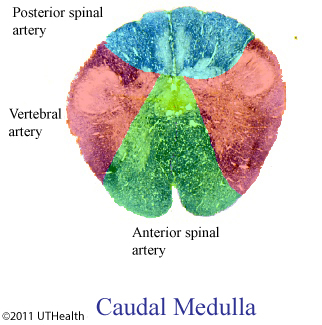
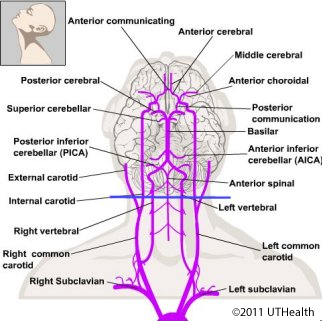
Review the relationships between arteries and the regions supplied by them using the figures. The figure on the right shows cross sections of the brainstem along with the arterial supply. Use the figure on the right to refer to the gross anatomy of the vasculature. Interruption of this vasculature causes vascular syndromes of the brainstem. These are listed here in order of frequency and are described below.
Medial Medullary (Alternating Hypoglossal Hemiplegia) Syndrome
Branches of the anterior spinal artery supply medial regions of the medulla. Occlusion of these branches or the anterior spinal artery produces the medial medullary or alternating hypoglossal hemiplegia syndrome. The deficits include a loss of discriminative touch and proprioception on the entire contralateral body area, a contralateral hemiplegia with positive Babinski sign, and paralysis of the ipsilateral half of the tongue. The structures involved include the medial lemniscus, the pyramids, and the hypoglossal nerve root. Notice that one symptom is on the side ipsilateral to the infarct (paralysis of the tongue with hypoglossal nerve loss) and that the other symptoms are on the contralateral side (corticospinal and medial lemniscus loss). The involvement of the hypoglossal nerve helps localize the site of damage.
Lateral Medullary or Wallenberg's Syndrome
Branches of the posterior inferior cerebellar artery (PICA) supply lateral regions of the medulla. Occlusion of the PICA produces the lateral medullary (or Wallenberg's) syndrome that is the most commonly occurring of the brainstem syndromes. Depending on the level of occlusion the deficits may include a loss of pain and temperature sensation on the entire contralateral body area; a loss of pain and temperature sensation on the ipsilateral face area; difficulty in swallowing and phonation; ipsilateral hearing deficit, nystagmus, nausea, ataxia toward the side of the lesion; and ipsilateral ptosis and miosis (Horner's syndrome) and decreased sweating. The structures involved include the spinothalamic tract, spinal trigeminal nucleus and tract, nucleus ambiguous, cochlear nuclei, vestibular nuclei, inferior cerebellar peduncle, and autonomic fibers descending through the area of the lesion. Horner's syndrome (ptosis, i.e., drooping of the upper eyelid; miosis, i.e., chronic pupil constriction; and decreased sweating) results from the interruption of fibers from the reticular formation or hypothalamus that normally descend to the thoracic spinal cord where they terminate on preganglionic sympathetic neurons in the lateral horn. The preganglionic axons exit the spinal cord and terminate in the superior cervical ganglion that sends its axons to the head. Depending on the speed and severity of the vascular insult, all or some of the symptoms may be transient or permanent.
Pontine Vascular Syndromes
There are a series of syndromes that result from thrombosis of the small vessels that supply the pons. These syndromes occur in many different combinations. Interruption of the blood supply to the anteromedial region of the pons through the paramedian branches of the basilar artery causes ipsilateral flaccid paralysis of the lateral rectus muscle, internal strabismus and inability to deviate the eye laterally because of involvement of rootlets of the abducens nerve that are passing through medial areas of the basilar pons. There might also be a contralateral hemiplegia of the upper and lower extremities, hyper- reflexia, and Babinski sign from the involvement of the corticospinal fibers in the basilar pons. Notice that the one component of the paralysis is on the side ipsilateral to the infarct (abducens loss) and that the other component is on the contralateral side (corticospinal loss), which helps localize the lesion. If the medial lemniscus were involved, there would be loss of discriminative touch and proprioception from the contralateral body.
The short circumferential branches of the basilar artery supply the anterolateral regions of the pons, posterior to the distribution of the paramedian branches. The regions served by these short circumferential branches include the anterior edge of the pons tegmentum (i.e., the medial lemniscus, spinothalamic tract and facial nerve as it exits the brain stem). Interruption of this blood supply causes symptoms of flaccid paralysis and atrophy of the muscles of the ipsilateral face and loss of taste sensation from the anterior two thirds of the ipsilateral tongue from involvement of the facial nerve roots. The involvement of large parts of the middle cerebellar peduncle would result in some ataxia (loss of coordination occurring in the absence of paresis, rigidity, spasticity or involuntary movement) ipsilateral to the lesion.
The long circumferential branches of the basilar artery and superior cerebellar artery supply posterolateral regions of the pons, including the superior cerebellar peduncle, the entering trigeminal root fibers, the mesencephalic and main sensory trigeminal nuclei, the trigeminal motor nucleus, and the spinothalamic tract. Occlusion of these arteries would cause ipsilateral cerebellar signs (superior cerebellar peduncle); anesthesia of the ipsilateral face (entering trigeminal root fibers); paralysis and atrophy of the ipsilateral muscles of mastication (trigeminal motor nucleus and trigeminal root fibers); and loss of pain and temperature sensation from the contralateral body (spinothalamic tract). Injury to the trigeminal root would also interfere with the afferent limb of the corneal reflex. The cerebellar signs would include intentional tremor, ataxia, myoclonus (rapid contractions of a muscle or muscle group), decomposition of movement, hypotonia, hyporeflexia.
Midbrain Vascular Syndromes
The paramedian branches of the basilar artery and proximal parts of the posterior cerebral artery supply the anteromedial regions of the midbrain base, including medial areas of the crus cerebri and substantia nigra; the exiting fibers of the oculomotor nerve and, in some cases, anterior areas of the red nucleus. The symptoms that result from occlusion of these vessels are often called Weber's syndrome and include a contralateral hemiplegia (or hemiparesis) of the extremities and Babinski's sign (corticospinal fibers in the crus cerebri); contralateral paresis (or paralysis) of facial expression on the contralateral lower face and deviation of the tongue to the contralateral side on protrusion (corticobulbar fibers to the facial motor nucleus and the hypoglossal nucleus); ipsilateral paralysis of most extraocular muscles, external strabismus, and ptosis of the eyelid, dilated pupil and absence of pupillary light reflex (oculomotor nerve roots).
The corticobulbar input to the motor neurons innervating the lower face are predominantly contralateral while those to the motor neurons innervating the upper face are bilateral. This is the reason that the contralateral lower face is affected and not the entire contralateral face. The tongue deviates ipsilateral to a lesion of the hypoglossal nerve.
If there is involvement of the red nucleus and adjacent cerebellothalamic fibers of the superior cerebellar peduncle, there may also be contralateral cerebellar signs.